What is a Behavioral Health Crisis?
Behavioral health crisis refers to any event or situation associated with real or potential disruption of stability and safety as a result of behavioral health issues or conditions. Crisis, as used here, does not only refer to situations that require calling 911 or 988. A crisis may begin at the moment things begin to fall apart (e.g., a person runs out of psychotropic medication and cannot obtain more, or is overwhelmed by urges to use substances they are trying to avoid) and may continue until the person is safely re-stabilized and connected or re-connected to ongoing supports and services. Crisis requests may be initiated by an individual, a caregiver or a service provider, as well as by any concerned person observing someone in need. Crisis systems and services should ideally be positioned to respond to any type of crisis request as soon as possible to prevent deterioration and for as long as necessary to help people in need stay safe and keep making progress, just like other community services.
What is a Behavioral Health Crisis System?
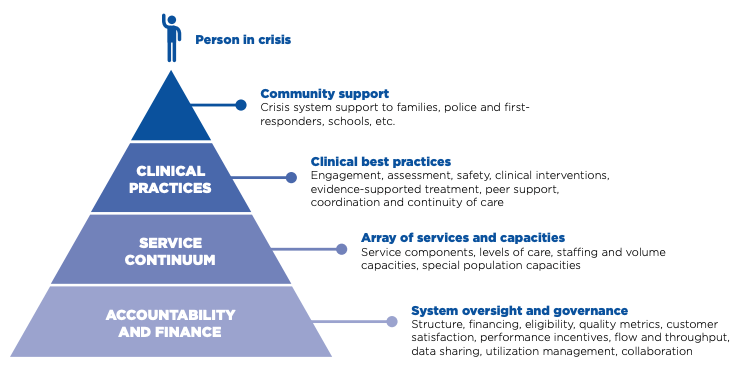
A behavioral health crisis system is more than a single crisis program, such as a mobile crisis team, a psychiatric emergency service or a crisis residential unit, and more even than just a few of those distinct elements. The term refers to an organized set of structures, processes and services that are in place to meet all the urgent and emergent behavioral health crisis needs of a defined population in a community, as soon as possible and for as long as necessary. In short, a crisis system involves an array or continuum of components, processes and services managed collaboratively and interlinked.
The target population for the system of services is ideally defined geographically, as a state, county, multi-county region or city, although other mechanisms (e.g., covered lives) may be used at times. Successful systems require multiple layers of organization and partnership based on ongoing collaborations within the community to address the behavioral health crisis needs of the population of the community
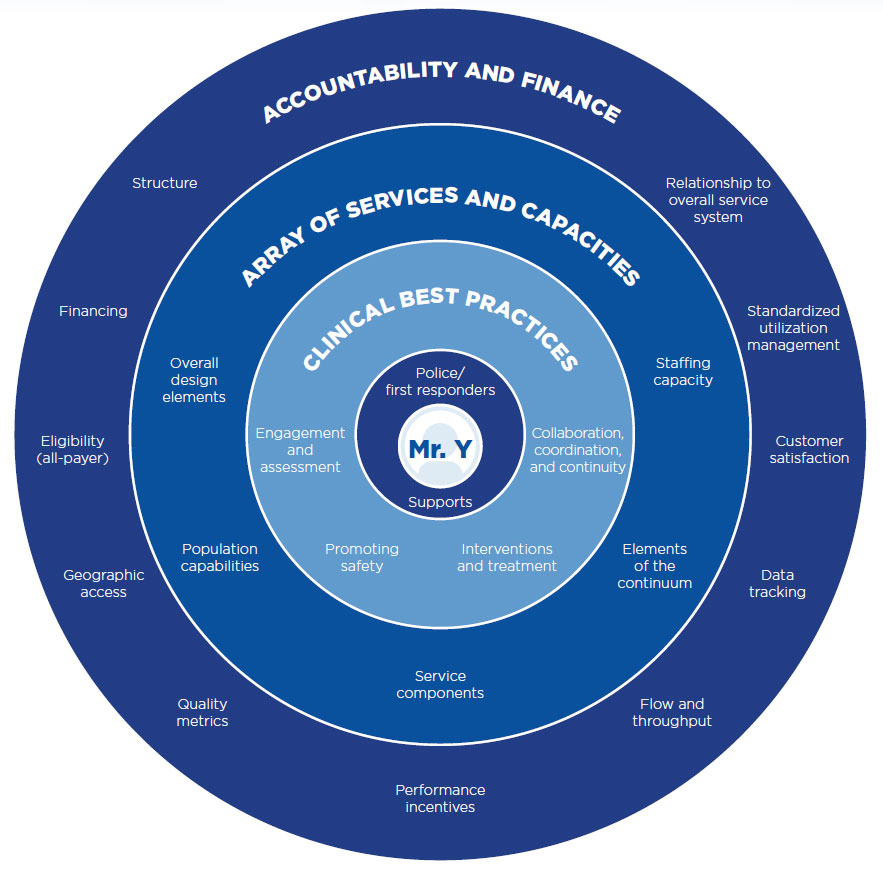
The concept of a crisis system in this report is intended to be distinguished from the routine system of short-term or ongoing care, although the two must necessarily interact seamlessly for service users and providers alike. Even an ideal crisis system cannot succeed without adequate access to good quality routine care to hand people off to once their crisis is resolved and to meet the behavioral health needs of the majority of the community before they fall into crisis.
What is an Ideal Behavioral Health Crisis System?
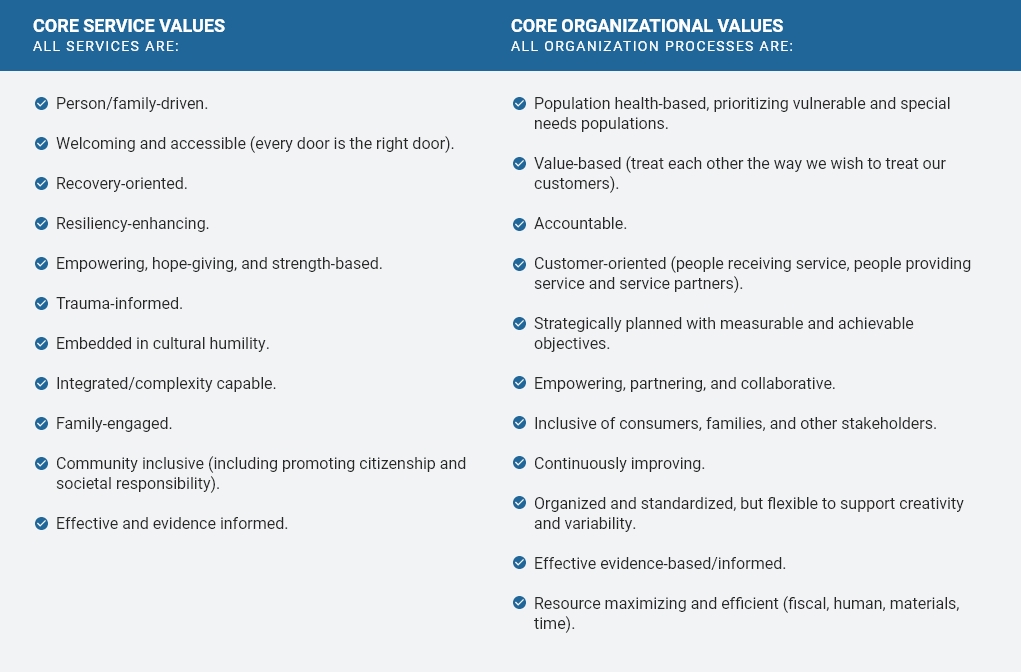
In an ideal behavioral health system, every individual and family with behavioral health issues can receive services that are helpful and effective quickly and easily for as long and as intensively as needed to achieve the best possible results for a successful and meaningful life. “Ideal” as used here does not mean perfect, nor does it assume unlimited resources. It refers to a set of recommendations or criteria any community can use to determine how to invest resources to achieve the best overall outcomes and to incorporate the known best practice processes, programs and practices that would contribute to the achieving the best possible results, as effectively, efficiently and flexibly as possible.
The Roadmap to an Ideal Crisis System
For communities across the US to transition from minimal behavioral health crisis services toward an ideal system, there must be a blueprint that contains all aspects of an ideal crisis system along with measurable performance criteria that communities can use for ongoing assessment of their progress through a continuous quality improvement process. The blueprint can provide a framework for community leaders (e.g., county executives, behavioral health system administrators, health system leaders, judges), funders (e.g., state agencies, Medicaid, commercial insurers, managed care organizations, accountable care organizations, counties, cities, community foundations) and other stakeholders (e.g., behavioral health providers, other human service providers, emergency responders, law enforcement, people and families receiving services) to come together to develop a shared vision of an excellent crisis system for their community, a set of shared values and action steps for making progress.
This report describes the criteria of an ideal behavioral health crisis system as a blueprint for any community to follow to establish community crisis services for individuals and families with mental health and substance use needs that are on par with other essential community services that respond to other types of crises.
